Revenue teams spend hours every day handling the same patient calls. Questions about insurance, payments, appointments, and billing come in nonstop. At the same time, patients get stuck in phone menus, abandon calls when they can’t reach anyone, and delay payments because they don’t get answers when they need them. The result is lost revenue, higher costs, and lower patient satisfaction.
AI voice agents for healthcare change how these conversations happen. Instead of routing patients through rigid phone trees, AI agents understand natural speech, medical terms, and insurance details. They respond instantly, guide patients to the right outcome, and resolve common issues without handoffs.
These agents can manage thousands of conversations at once while still feeling personal and responsive. That combination makes it easier for patients to get help and easier for revenue teams to operate efficiently.
AI voice agents are improving healthcare revenue in three key areas: automating payment collection, reducing no-shows, and handling insurance verification around the clock. This guide breaks down the revenue impact, what to look for when choosing a platform, and how connecting voice AI to a centralized CRM helps drive measurable ROI.
Key takeaways
- Replace frustrating phone menus with natural conversations: AI voice agents understand spoken requests and provide personalized responses, leading to higher patient satisfaction and completed interactions.
- Automate payment collections and reduce no-shows: voice agents handle payment reminders, explain bills, and confirm appointments proactively, directly improving cash flow and appointment fill rates.
- Centralize voice interactions with revenue operations on modern platform: track every patient touchpoint in one place and automate follow-up workflows based on conversation outcomes for maximum revenue impact within solutions like monday CRM.
- Choose platforms that integrate seamlessly with your existing systems: evaluate EHR connections, billing system compatibility, and customization capabilities to avoid data silos and workflow disruptions.
- Focus on measurable ROI through systematic implementation: map current bottlenecks, calculate total costs, and track performance metrics like collection rates and patient satisfaction to maximize your voice AI investment.

How do AI voice agents create value for healthcare revenue teams?
AI voice agents engage patients in natural, human-like conversations. Unlike traditional phone systems that force patients through rigid button-press menus, these platforms understand what patients say and respond with the right information. The tech recognizes voices, understands medical terms, and talks to patients in ways that actually help.
For revenue teams, AI voice agents deliver measurable financial advantages over traditional systems.
This technology maintains patient engagement throughout interactions, resulting in higher call completion rates, improved appointment attendance, and more timely payment collection.
AI voice agents also adapt to each patient’s specific needs, understand medical terminology and insurance concepts, and provide accurate responses without complex menu navigation, leveraging conversational AI technology. The outcome is improved operational efficiency: patients complete their calls with accurate information exchange, attend scheduled appointments, and fulfill payment obligations consistently.
The advantages of AI voice agents over traditional IVR
Traditional IVR systems make patients guess which menu option fits their question before they can get help. AI voice agents eliminate this friction by understanding natural requests. When a patient says “I received a bill but my insurance should have covered this procedure,” the system provides detailed, personalized guidance that addresses their specific situation.
The technical differences translate into practical advantages:
- Conversation flow: AI agents dynamically navigate conversations by asking relevant questions and directing patients to the information they need. Traditional systems require patients to navigate through predetermined menu options in a fixed sequence.
- Understanding capability: AI agents recognize context and intent, understanding that “I need to reschedule” and “Can I move my appointment to next week?” express the same request, unlike keyword-based systems that fail with different terminology.
- Response quality: AI agents access patient history and account details to provide personalized responses tailored to individual circumstances, rather than delivering generic scripted messages.
- Error handling: when AI agents encounter unclear input, they rephrase questions and attempt alternative approaches to understanding patient needs, rather than terminating the interaction.
Natural language processing in medical conversations
Natural language processing enables AI voice agents to understand specialized vocabulary and complex concepts inherent in healthcare conversations. The technology processes patient speech instantly, accurately identifying medical terms and insurance details with high precision.
Healthcare-trained NLP means voice agents handle medical conversations that trip up regular AI. When a patient says “My copay was supposed to be $30 but I was charged $150,” the system understands insurance terminology, accesses the patient’s coverage details, identifies the billing discrepancy, and provides an explanation based on actual policy terms and claim processing.
- HIPAA-compliant processing: ensures patient information remains secure throughout these interactions, with voice data encrypted during transmission and storage.
Real-time learning and adaptation
AI voice agents improve continuously through each patient interaction, building knowledge about communication preferences, common questions, and optimal response patterns. The systems track what explanations help, what confuses people, and what gets patients to follow through.
Voice agents adapt based on who they’re talking to and what’s happening in the conversation:
- Confusion detection: when a patient sounds confused, the system gives more detail.
- Urgency recognition: it picks up on urgency and bumps those requests to the front.
- Personalized context: for returning patients, it remembers past conversations and gets better every time.
AI voice agents boost revenue by automating calls, making payments and scheduling easier, and keeping patients happy enough to stick around and refer others. Each change creates a measurable way to make more money.
7 ways AI voice agents transform healthcare revenue operations
1. Automate payment collections and financial counseling
AI voice agents handle every part of payment conversations. They send payment reminders, explain bills, set up payment plans, and answer insurance questions.
The revenue impact manifests in three key areas:
- Collection costs: automated calls cost significantly less than staff time or collection agencies.
- Payment acceleration: patients can arrange payment immediately during the call, reducing days sales outstanding.
- Compliance improvement: clear explanations and flexible payment options increase payment completion rates.
2. Improve appointment attendance with intelligent scheduling
AI voice agents reduce no-show rates by contacting patients through their preferred communication channels at optimal times. These systems provide comprehensive appointment management that extends beyond simple confirmation; they identify scheduling conflicts, offer alternative appointment times immediately, and deliver strategic reminders as appointments approach.
No-show rates decrease significantly when AI identifies high-risk patients based on historical attendance patterns, demographic factors, and appointment characteristics. These patients receive enhanced engagement through:
- Multiple reminder touchpoints: patients receive confirmation calls, text reminders, and follow-up messages at strategic intervals before their appointments.
- Transportation assistance information: voice agents proactively provide details about transportation options, parking, and accessibility resources to remove logistical barriers.
- Direct staff follow-up when needed: high-risk cases automatically escalate to human staff members who can address specific concerns and provide personalized support.
3. Accelerate insurance verification and prior authorizations
AI voice agents call patients before appointments to confirm coverage, get documents, and collect info for prior authorizations. The systems chase down pending authorizations, update patients on approvals, and reschedule when things get delayed.
- Revenue impact: faster approval processes and reduced administrative burden. Staff spend less time on verification calls and more time on work that matters. Revenue comes in faster when procedures don’t wait on authorizations.
4. Streamline patient intake and registration
AI voice agents collect patient info, insurance details, medical history, and consent forms before appointments. The systems guide patients through the info step by step, check accuracy, and upload forms straight to the EHR.
Revenue improvements manifest through:
- Increased appointment capacity: when check-in takes two to three minutes instead of ten to 15 minutes, practices can schedule appointments closer together without creating waiting room congestion.
- Improved data quality: more accurate patient information leads to cleaner claims and fewer denials from demographic or insurance errors.
5. Enable 24/7 medication refill processing
AI voice agents process medication refill requests outside regular business hours, integrating with pharmacy systems and addressing insurance inquiries without requiring staff intervention. Patients can request refills at any time through natural conversation, receiving immediate confirmation of their requests.
This capability delivers measurable revenue benefits through improved patient retention. Patients who experience convenient prescription management demonstrate higher practice loyalty and generate referrals.
Additionally, these systems identify medication non-adherence patterns and initiate proactive outreach — a critical function for value-based care contracts where adherence metrics directly influence reimbursement rates.
6. Conduct post-discharge follow-ups at scale
AI voice agents conduct automated follow-up calls after discharge to assess patient recovery, medication adherence, and care plan compliance. These systems inquire about symptoms, side effects, and patient concerns, escalating issues that require clinical attention to appropriate healthcare providers.
- Revenue protection: reduced readmissions and improved outcomes that support value-based care contracts. Regular follow-up catches problems early so patients get outpatient care instead of hitting the ER, avoiding penalties and payment cuts.
7. Handle multilingual patient communications
Real-time translation lets AI voice agents talk to patients in dozens of languages without requiring multilingual staff or interpreters. The systems pick up on language preference and switch automatically without breaking the flow.
- Revenue expansion: improved access for diverse patient populations. Healthcare organizations in multilingual communities can serve patients who previously faced language barriers, expanding their potential patient base through improved lead generation while reducing interpreter costs that typically run significant hourly rates.
5 steps to select the right healthcare voice AI platform
Selecting the right voice AI platform requires a systematic evaluation of how the technology addresses your specific revenue challenges, integrates with your existing systems, and delivers measurable returns. This framework guides you through the selection process, helping you identify the platform that best fits your organization’s needs while avoiding costly implementation pitfalls.
Step 1: map your revenue cycle bottlenecks
Revenue cycle analysis shows you which communication problems hurt cash flow and slow down operations. Start by putting numbers on your bottlenecks: unfilled appointment slots, slow payment collections, and insurance verification delays that hold up care and create denials.
For each bottleneck, track three things:
- Current volume: calls per day, transactions per month.
- Staff time required: minutes per interaction, FTE allocation.
- Financial impact: lost revenue, delayed collections, operational costs.
These numbers build your business case and give you a baseline for tracking success.
Step 2: evaluate integration with existing systems
Integration determines whether voice AI data connects to your revenue systems or gets stuck in silos. Map every system that needs to talk to voice agents: EHRs for patient info, billing systems for payments, and CRMs for relationship tracking.
API capabilities differ a lot between platforms:
- Pre-built connectors: some offer ready-made integrations for major healthcare systems like Epic, Cerner, and Athenahealth.
- Custom development: others require custom API development for integration.
- Maintenance requirements: check the technical work needed for setup and maintenance.
Step 3: assess customization without code requirements
Configuration flexibility shows whether voice agents fit your workflows or make you change how you work. Check if admins can change how voice agents handle scenarios without needing tech skills.
Voice agents should follow your policies for:
- Appointment scheduling: configuring availability rules, provider preferences, and booking protocols.
- Payment arrangements: setting payment plan terms, discount policies, and collection procedures.
- Insurance verification: defining coverage confirmation steps and documentation requirements.
- Clinical triage: establishing symptom assessment protocols and escalation criteria.
Platforms that require vendor involvement for protocol updates create dependencies and delays. No-code customization lets admins adjust voice agents when policies change.
Step 4: compare total cost of ownership
Voice AI pricing varies a lot, and your costs depend on how much you use it. Per-interaction pricing charges per call, so costs go up and down with volume. Monthly subscription models provide predictable costs but may include usage caps that trigger overage charges.
Calculate ROI by comparing total costs to the benefits you mapped earlier. Include all cost categories:
- Platform licensing: subscription fees or per-interaction costs for the voice AI service.
- Implementation services: initial setup, configuration, and deployment support from the vendor.
- Ongoing support: technical assistance, troubleshooting, and platform updates.
- System integration: connecting voice AI to your EHR, billing systems, and other tools.
- Staff training: educating team members on managing and optimizing voice agents.
- Internal resources: staff time dedicated to ongoing management and optimization efforts.
Step 5: verify healthcare-specific track record
Vendor experience with healthcare clients shows the platform’s ready for your needs and lowers implementation risk. Request references from organizations with similar size, patient volume, and use cases.
Verify vendor claims about HIPAA compliance through thorough due diligence:
- Request recent third-party security audits: obtain documentation of independent security assessments conducted within the past year.
- Review penetration testing results: examine vulnerability testing reports to understand potential security weaknesses.
- Verify compliance certifications: confirm current HIPAA, HITRUST, or SOC 2 certifications are active and up-to-date.
- Examine business associate agreement terms carefully: standard vendor BAAs often favor the vendor and may not provide adequate protection for your organization.

Integrating voice AI with your healthcare tech stack
Integration determines whether voice AI fits your workflows or creates disconnected processes that need manual data transfer. Good integration means voice data goes straight to the systems your revenue team uses. These integration points matter most:
EHR synchronization requirements
Two-way data flow between voice agents and EHRs lets agents pull patient info during calls and update records after. Patient data access includes demographics, insurance details, appointment history, and relevant clinical information needed to personalize conversations.
Appointment scheduling integration allows voice agents to view available slots, book appointments directly, and send confirmations without staff involvement. The integration must respect:
- Provider preferences: individual clinician availability, booking restrictions, and scheduling requirements.
- Appointment types: visit categories, duration requirements, and resource allocation needs.
- Scheduling rules configured in the EHR: organizational policies, buffer times, and appointment sequencing protocols.
CRM data flow for patient relationships
Voice interactions generate valuable relationship data that extends beyond individual transactions. Conversation logging captures what patients ask about, concerns they express, preferences they indicate, and satisfaction signals they provide.
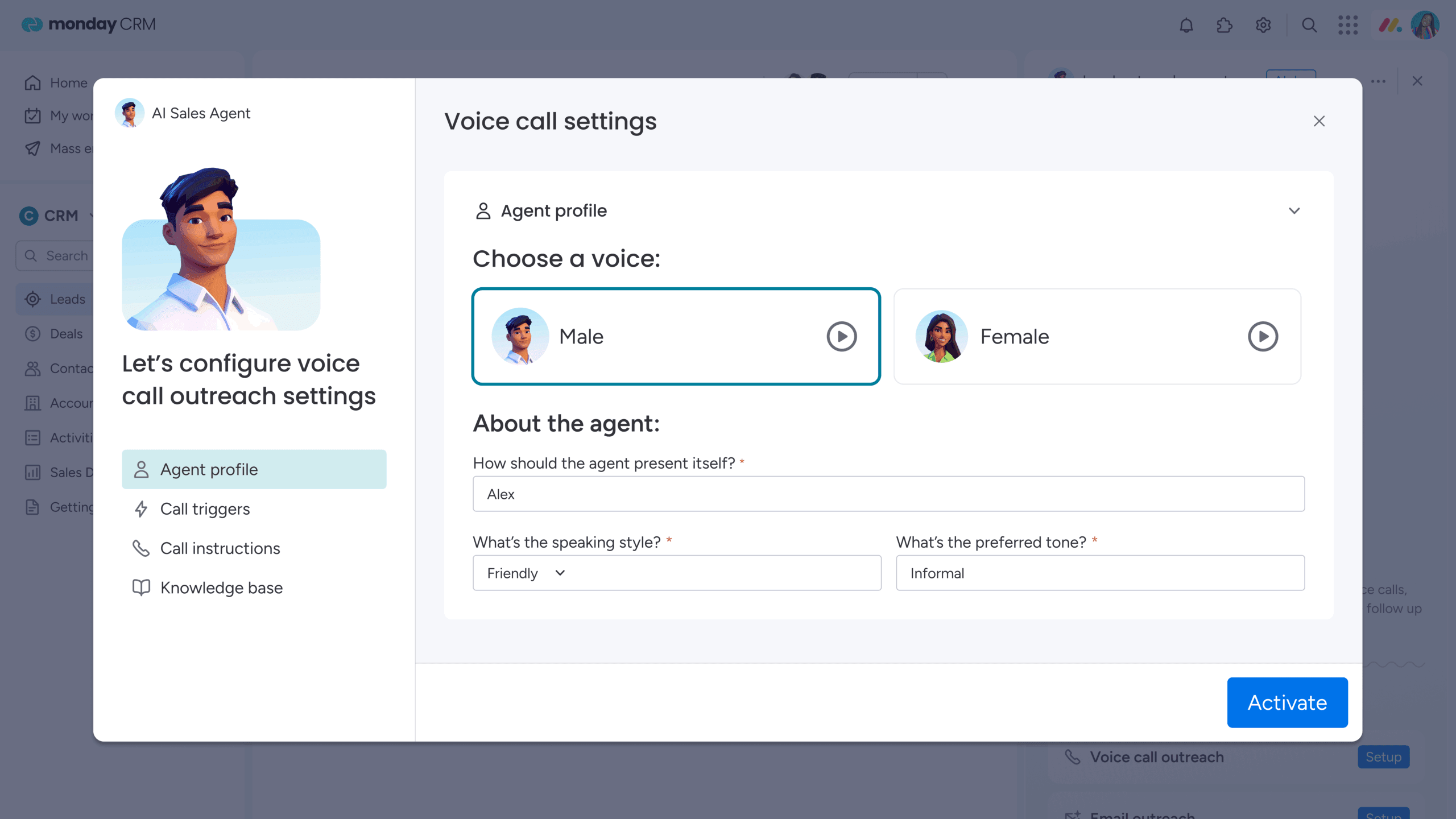
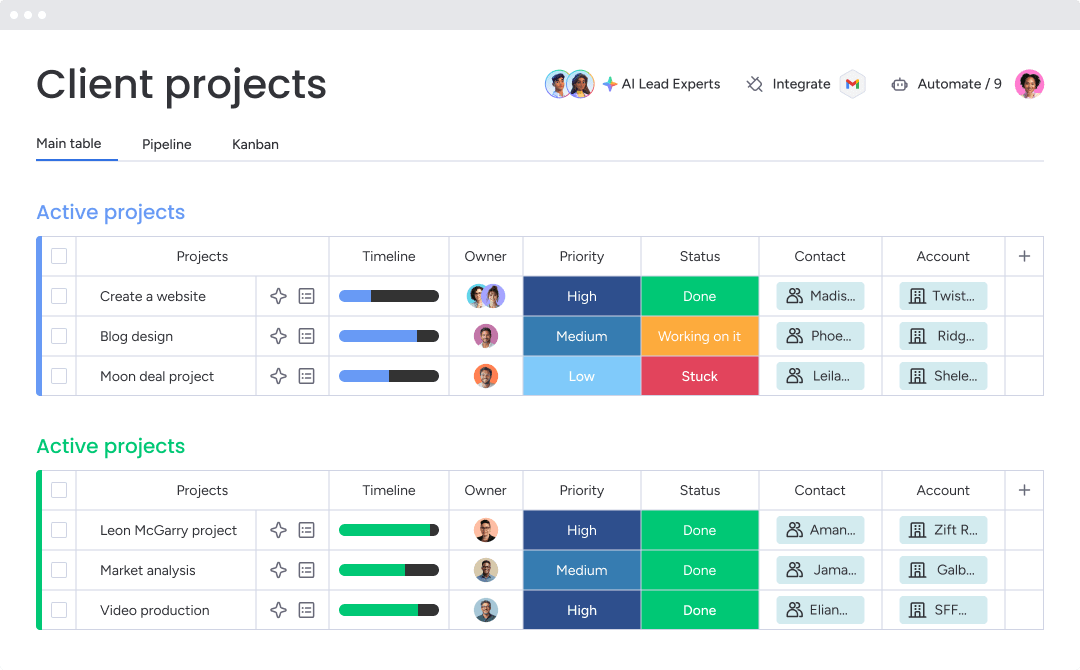
Revenue teams using platforms like monday CRM can centralize these patient touchpoints alongside other revenue cycle activities, creating comprehensive visibility into each patient’s journey from initial contact through ongoing care. The platform’s Emails & Activities feature logs and tracks every interaction including emails, meetings, and notes in one timeline, ensuring voice interaction insights inform staff actions and care coordination efforts through CRM agent capabilities.
Revenue cycle management system connections
Integration with billing systems enables voice agents to access account information, process payments, and update financial records during patient conversations. Real-time account status access shows:
- Current balances: outstanding amounts owed by the patient across all accounts.
- Recent payments: transaction history showing payment dates, amounts, and methods.
- Payment plan terms: installment schedules, due dates, and agreed-upon payment amounts.
- Insurance claim status: submission dates, processing stages, and pending reimbursements.
Financial workflow automation triggers based on voice interaction outcomes. When a patient commits to a payment plan, the system creates the plan automatically and schedules future payment reminders.
The automation capabilities in monday CRM can route these follow-up actions to appropriate team members based on interaction type and content, ensuring the right person handles each follow-up at the right time.

Turn AI voice interactions into revenue with centralized tracking
AI voice agents generate valuable patient interaction data, but this data only drives revenue when it flows into systematic workflows for tracking, follow-up, and optimization. Most healthcare organizations face a critical gap where voice interactions occur in one system while revenue operations happen in another. Centralized tracking bridges this gap and transforms voice interactions into measurable revenue outcomes.
Centralize every patient touchpoint
Voice interaction data gets captured automatically through integrations with AI voice platforms in monday CRM, organizing conversations alongside other patient communications in unified patient journey boards. Each patient record shows the complete interaction history including voice calls, emails, portal messages, and in-person visits.
The platform’s customizable fields capture healthcare-specific data from voice interactions:
- Insurance verification status: current coverage confirmation and authorization tracking.
- Payment arrangement terms: installment schedules, amounts, and commitment dates.
- Appointment preferences: preferred times, providers, and visit types.
- Communication preferences: preferred contact methods and optimal outreach times.
Revenue teams can filter and sort patients based on any field, identifying everyone who needs insurance follow-up or everyone with payment plans.
Automate follow-up workflows with AI
AI capabilities provided by solutions like monday CRM process voice interaction summaries to extract key information, categorize patient needs, and trigger automated follow-up sequences. The AI blocks feature can detect sentiment, extract information from documents, and assign labels automatically based on conversation content.
Automated task assignment routes follow-up actions to appropriate team members based on interaction type and content:
- Billing questions: go to financial counselors.
- Clinical questions: go to the nursing staff.
- Assignment rules: consider staff specialization and current workload, ensuring the right person handles each follow-up.
Track performance with revenue dashboards
Dashboard capabilities in monday CRM provide real-time visibility into voice AI ROI, patient conversion metrics, and revenue cycle performance. Revenue teams see how voice interactions impact key outcomes including appointment fill rates, payment collection percentages, and patient satisfaction scores.
The platform’s sales-specific widgets like the leaderboard and funnel help identify strong and weak points in your pipeline. These dashboards update automatically as voice interaction data flows into the platform, providing current performance visibility without manual reporting.
“With monday CRM, we’re finally able to adapt the platform to our needs — not the other way around. It gives us the flexibility to work smarter, cut costs, save time, and scale with confidence.”
Samuel Lobao | Contract Administrator & Special Projects, Strategix
“Now we have a lot less data, but it’s quality data. That change allows us to use AI confidently, without second-guessing the outputs.”
Elizabeth Gerbel | CEO
“Without monday CRM, we’d be chasing updates and fixing errors. Now we’re focused on growing the program — not just keeping up with it."
Quentin Williams | Head of Dropship, Freedom Furniture
“There’s probably about a 70% increase in efficiency in regards to the admin tasks that were removed and automated, which is a huge win for us.“
Kyle Dorman | Department Manager - Operations, Ray White
"monday CRM helps us make sure the right people have immediate visibility into the information they need so we're not wasting time."
Luca Pope | Global Client Solutions Manager at Black Mountain
“In a couple of weeks, all of the team members were using monday CRM fully. The automations and the many integrations, make monday CRM the best CRM in the market right now.”
Nuno Godinho | CIO at VelvMaximize your voice AI investment with integrated revenue operations
Healthcare organizations that successfully implement AI voice agents see the greatest returns when they connect voice interactions to comprehensive revenue cycle management. The technology transforms patient communication, but the real value emerges when those interactions drive systematic follow-up, performance tracking, and continuous optimization.
Voice AI platforms generate rich interaction data that reveals patient preferences, payment patterns, and communication effectiveness. Organizations using monday CRM to centralize this data alongside other revenue activities create a complete view of each patient’s journey and can optimize every touchpoint for maximum revenue impact.
The combination of intelligent voice interactions and systematic revenue operations creates a competitive advantage that extends beyond cost savings to include improved patient satisfaction, increased retention, and expanded market reach through multilingual capabilities.
Frequently asked questions
How much do healthcare AI voice agents typically cost?
Healthcare AI voice agent costs typically range from $0.05-$0.50 per interaction for usage-based pricing, $500-$5,000 monthly for subscription models depending on call volume, or $50,000-$500,000 annually for enterprise licenses with unlimited usage.
What languages can AI voice agents support for patient care?
Most healthcare AI voice platforms support 20-100 languages with real-time translation capabilities, including Spanish, Mandarin, Vietnamese, Korean, and Arabic, with cultural adaptation beyond literal translation.
How long does voice AI implementation take in healthcare settings?
Voice AI implementation typically takes six to sixteen weeks from contract signing to production deployment, including system integration, conversation flow development, staff training, and pilot testing.
Can AI voice agents handle medical emergencies?
AI voice agents include emergency protocols that recognize urgent symptoms and escalate immediately to human staff or emergency services, but they are not designed to replace emergency response systems.
Which medical specialties see the highest ROI from voice AI?
Primary care, orthopedics, and chronic care management see the highest ROI from voice AI due to high patient communication volume and routine interactions that automate well.
How do you measure success with healthcare voice agents?
Success metrics include patient satisfaction scores, operational efficiency measurements like staff time saved, revenue cycle improvements such as reduced no-show rates and faster payment collection, and cost reduction calculations comparing voice AI costs to previous manual processes.